Foreword
Main Article Content
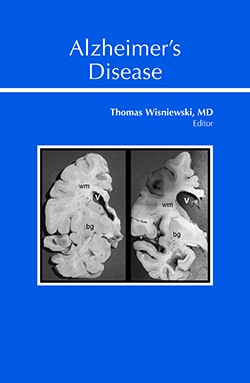
Alzheimer’s disease (AD) is the sixth leading cause of death in the USA. Globally about 50 million individuals have AD or related dementias. With the increasing average age of humans worldwide, the total number of people with dementia is projected to reach 82 million by 2030 and 152 million by 2050. Despite its prevalence, AD is the only cause of death among the top 10 causes of death globally for which no effective pharmaceutical agents exist to halt or slow down the disease progression. By some estimates, AD and related dementias are the single most expensive medical condition. In 2019, direct costs of AD in the USA will be ~$290 billion, which is expected to rise to ~$1.1 trillion by 2050 if no treatments are developed. Hence, there is a tremendous imperative to gain a better understanding of the pathogenesis of AD and to develop effective treatments. AD is a complex, multifactorial disease, which is unique to humans. AD is defined neuropathologically by the accumulation of amyloid β (Aβ) into extracellular plaques in the brain parenchyma and in the vasculature (known as congophilic amyloid angiopathy [CAA]), and abnormally phosphorylated tau that accumulates intraneuronally forming neurofibrillary tangles (NFTs). Pathological aggregation of phosphorylated tau and Aβ occurs in a sequential process. Monomers first aggregate into oligomers intraneuronally that then further aggregate into the fibrils observed in amyloid plaques and NFTs. This pathology then spreads in a characteristic brain topography that is distinct for NFTs and plaques. This process develops over many years, with a preclinical period of two to three decades, the onset of which is modulated by apolipoprotein E (apoE) genotype, as well as other genetic and environmental risk factors. CONTINUE READING.....
Downloads
Metrics
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.